Introduction:
The following information is a guide to your upcoming surgery. It describes what is likely to happen at your upcoming surgery. This is a guide only and there may be some individual variation depending on your individual circumstances. Dr Lawrie will discuss these with you. Please become familiar with this guide and discuss any aspects you wish to with your surgeon, anaesthetist and/or nursing staff. You will be admitted to the ward either on the morning of your surgery or the night before, depending on the time of day of your surgery. A typical hospital stay is 3-7 days. You will be able to travel home in your own vehicle, but you cannot drive for at least six weeks.
Knee Replacement Surgery:
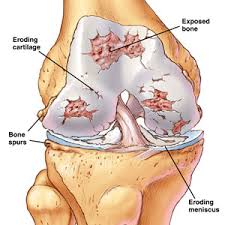
With age and also with rheumatoid arthritis the weight bearing surface of the knee is worn away; they are no longer smooth and free which leads to stiffness and pain. Eventually the joint wears away to the point that the bone on the femur grinds on the tibia. The kneecap is commonly involved as well. As the bone becomes more worn away and bony spurs start to form, the knee becomes out of shape and deformed.
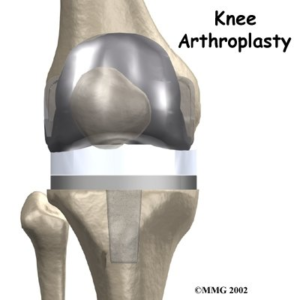
A total knee replacement replaces these surfaces with plastic and metal. The femur replacement is a smooth metal component that fits snugly over the end of the femoral bone. The tibial component is in two pieces; a titanium base plate that attaches to the bone and a hard plastic bearing surface that snaps into the base plate. The smooth metal femoral component glides on the hard plastic tibial bearing. If necessary the patella is replaced or resurfaced with a hard plastic dome, which glides on a groove in the femoral component. Often the patella does not need replacing.
 Before Surgery
Before Surgery
You should stop anti-inflammatory drugs at least five days prior to surgery as they can increase the chance of bleeding (e.g. Voltaren, Naprosyn, Nurofen, Brufen, Feldene and Indocid). Celebrex and Mobic are not a problem. It is extremely important that you have no cuts, scratches or sores on your lower limb at the time of surgery as these can increase the chance of infection. If you have any scratches or cuts then your surgery will be postponed until they are well and truly healed. Please contact Dr Lawrie’s rooms well before your surgery day if you notice any of these problems or have any concerns.
Postponing the surgery on the day of your operation is very distressing for all concerned. If this can be done ahead of time the theatre time may be used for another patient and resources can be redirected. There is a lot of logistical work that goes into a joint replacement, this will be lost if the operation is postponed on the day.
On the day of surgery a nurse will inspect your leg for lesions. The nurse will use clippers to remove long hair from the knee and dress the knee with an antiseptic solution. Dr Lawrie will also inspect the leg and mark the appropriate leg with an indelible marking pen.
Admission
You should not eat or drink for 6 hours prior to surgery. You should bring with you:
- Personal effects (nightgown or pyjamas, slippers, dressing gown, toiletries)
- Any medication you are taking
- All relevant x-rays, scans and reports
- Medicare and private health fund membership cards
- This paperwork
Prior to going to the operating room, the ward staff will direct you to:
- Have a shower with an antiseptic soap
- Be dressed in a theatre gown and disposable underwear
- Have the limb inspected and dressed with an antiseptic solution and sterile drape
If you wish Dr Lawrie to speak to a family member after the operation please notify the nursing staff with contact details.
The Procedure
You will be taken into the operating room on a trolley by the nursing staff. The operation will take about 90-120 minutes but you may spend up to two and a half to three hours in the theatre complex. You will spend time in the pre-operative area; you will be prepared for your anaesthetic and then woken up in the recovery area.
The Anaesthetic
You will meet the anaesthetist prior to your admission when he will discuss with you the different anaesthetic options. The type of anaesthetic you have will be tailored to your needs, taking into account any medical conditions you may have. You may be given a general anaesthetic (where you are completely asleep) or a regional anaesthetic such as an epidural or spinal anaesthetic where the nerves to the limb are numbed from a needle placed into your back.
A combination of spinal anaesthesia and local anaesthetic infiltration into the knee joint works best for the majority of patients. This gives very good pain relief, safety under anaesthesia and allows for early mobilisation after surgery
The Surgery
You will be placed on the operating table lying on your back. A tourniquet will be placed around your thigh. You will be covered in sterile drapes with only the operation site exposed. Dr Lawrie will check your x-rays and use those to ensure that your new knee is placed in exactly the right place and at the right angle for your knee. Any deformities due to your knee condition can often be corrected by your new knee replacement.
An incision will be made over the front of the knee joint slightly towards the inner side of the knee. A typical incision is about 15-20cm long. This may be greater if more access is needed due to individual circumstances. Great care is taken to ensure that the major nerves and vessels about the knee joint are protected.
 The knee joint is opened and the deformity due to contracted soft tissue and bony spurs is corrected. The cruciate ligaments are assessed and released as necessary. Very accurate jigs are used to ensure the right sized component is used on the femur and tibia and/or patella (kneecap). Dr Lawrie has been using Computer Assisted Surgery (CAS) instead of traditional jigs since 2005 as the alignment device for Total Knee Replacement. This allows more accurate positioning of the knee replacement and feedback throughout the procedure to ensure all is going well and allow for any corrections that need to be made. (please see information sheet on CAS for further details).
The knee joint is opened and the deformity due to contracted soft tissue and bony spurs is corrected. The cruciate ligaments are assessed and released as necessary. Very accurate jigs are used to ensure the right sized component is used on the femur and tibia and/or patella (kneecap). Dr Lawrie has been using Computer Assisted Surgery (CAS) instead of traditional jigs since 2005 as the alignment device for Total Knee Replacement. This allows more accurate positioning of the knee replacement and feedback throughout the procedure to ensure all is going well and allow for any corrections that need to be made. (please see information sheet on CAS for further details).
Next the worn-out cartilage and bone is removed using the jigs. The ends of the bone are fashioned to perfectly fit the new components. Dummy components are placed to ensure that the new knee replacement is placed in the right alignment, the knee bends smoothly and the soft tissues that control knee movement are balanced. The patella is then inspected and if it is worn out then it too is replaced. The key to a good knee replacement is how well the patella sits in the new knee replacement. Many checks are made along the way to make sure the kneecap is moving appropriately.
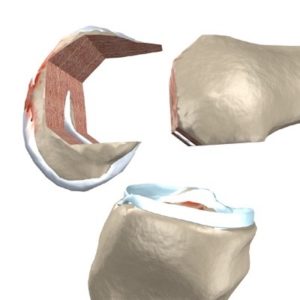
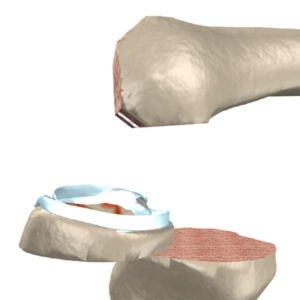
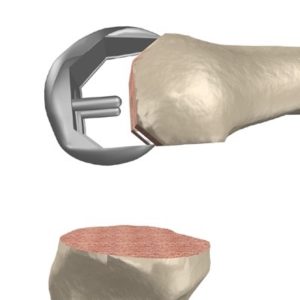
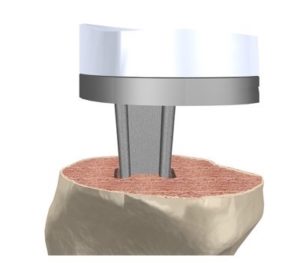
Once Dr Lawrie is happy that the dummy knee replacement is functioning properly then the real knee replacement is put in place. The tibial component is cemented in place. The cement acts to transfer forces to the tibial bone evenly from the knee replacement. The tibial component is a combination of a titanium based plate with a snap in bearing surface made of very hard plastic. The Femoral component is then cemented in place. This is made of a metal alloy of chrome-cobalt or of Oxinium a new alloy which has a very low wear rate as its surface has similar properties to ceramic without the risks of ceramic fracture. If the patella is being replaced it is then cemented into place; this is made of the same hard plastic as the tibial bearing.
A final check is made to ensure that the knee is functioning perfectly. The soft tissues of the knee are then repaired with sutures and a firm bandage is applied to the knee. Sometimes a drain is put in the knee to prevent bruising. Your anaesthetist will withdraw your anaesthetic. A catheter will be placed into your bladder at the end of the operation to prevent any problems with the bladder post-operatively.
The Recovery
You will be wheeled into recovery and the nurse will monitor your blood pressure, pulse and breathing as you recover from your anaesthetic. The nurse will check on the sensation and circulation of your limbs.
After Surgery
Dr Lawrie will see you following surgery to explain the operative findings and you will be given a copy of the operative report and a copy will be sent to your local doctor. After returning to the ward a drip will be placed into your arm; this will keep you well hydrated until you are eating and drinking normally.
Your blood level will be checked to determine whether you may need a blood transfusion. You will have tight stockings around both legs, which helps to prevent blood clots. These need to be worn for six weeks from the time of your surgery. Foot pumps will also be used to prevent blood clots. Your usual medications will be given to you and you will be placed on antibiotics through the drip for 24hrs to reduce the risk of infection. Aspirin will be added to your medications and you should continue to take this for six weeks from the time of surgery to help prevent clots.
Patients at high risk of blood clots will typically be placed on potent anti-clotting agents post-operatively. If you have had a blood clot previously or are aware of being at increase risk please ensure you have relayed this to all your treating doctors. You will be given morphine type medication for pain relief. This can make you drowsy and nauseated. Your anaesthetist will keep a close eye on your pain relief and will endeavour to keep you comfortable.
Commonly patients will be given a PCA (Patient Controlled Analgesia), which allows you to control the amount of painkiller that is administered through your drip. An x-ray will be taken of your knee following your surgery to check on the position of your components. Your blood level will be checked the following day. A physiotherapist will visit you following your surgery to look after your mobility following surgery.
The most important thing you can do on return to the ward is to get moving as soon as possible. This helps to prevent clots and to maximise your new knee’s flexibility and minimise muscle weakness post surgery. This starts with toe wiggling immediately after surgery and progresses quickly to standing out of bed and bending the knee the day of your surgery and walking with the aid of a frame or crutches a day or two following your surgery.
You will be given a number of exercises by the physiotherapist, which will aid in getting back your muscle strength and getting you back on your feet. You will be ready to leave when you can bend the knee to 90°, walk about 30 metres on your own, get in and out of bed, access the toilet and shower, and get up and down stairs successfully.
Your Physiotherapy
A knee replacement involves a lot of physiotherapy and a lot of hard work. Patients are often surprised at how hard it is to get their new knee working following surgery. If you are not mentally prepared for the hard work following surgery then it is very difficult to get your knee moving. The knee will be sore, despite the pain relieving medications, and you will have to work through the pain in order to get the pain to settle down.
Your exercises will start immediately after you return to the ward with wriggling of the toes. Depending on the time of day you return to the ward the physiotherapist will have you out of bed the day of your surgery as well as work on muscle strengthening and range of motion. This will continue throughout your stay. The knee will be sore despite the pain relieving medications and you have to work through the pain in order to get the pain to settle down. Regaining control of the quadriceps muscles at the front of you thigh is very important and the physiotherapists will continue to exercise this area.
The keys to a good result post-operatively are:
- getting control of your pain
- obtaining good quadriceps function
- then working on knee bending.
Your physiotherapy will continue when you go home and will continue for 6-12 weeks; depending on your progress.
When You Get Home
Mild pain in the knee is normal on returning home. The knee is often sore for the first 6-12 weeks. Simple painkillers such as Panadiene Forte should control this. Movement, swelling and pain should all steadily improve over the next 6-12 weeks. If any of these is not improving then contact Dr Lawrie.
Once you have had your knee replacement and completed your recovery your knee should have a range of motion of at least 100-120°. This should be sufficient for your routine daily activities such as walking and climbing stairs. Greater range of motion can be obtained in some cases. Knee replacement surgery usually gives excellent pain relief, with little or no pain. Most people with knee replacements can do recreational walking, swimming, golf, driving, light hiking, recreational biking, ballroom dancing and stair climbing without difficulty.
Patients with a knee replacement generally report excellent pain relief, but the knee does not feel like a new knee. There is often a feeling like there is nothing between the femur and the tibia, even though the knee is stable and pain free. This is a normal experience. The new knee often clicks as the knee moves and with weight bearing. There will be a numb patch of skin on the outside of the knee which is permanent. This is because the small nerves that supply the area must be cut by the incision needed to place the knee replacement.
Many patients are unable to kneel down on the replaced knee; however, some patients are able to kneel. Activities that require deep knee flexion, such as squatting on your haunches, are often not possible following knee replacement surgery. It is very important to treat any infections in other areas aggressively, such as urinary tract or dental infections. Many invasive procedures require antibiotics prior to the procedure.
It is always best to warn your doctor beforehand that you have had a knee replacement as the consequences of an infected knee replacement can be dire. Surgery on infected knee replacements is extremely difficult and is not always successful at eradicating the infection. One can be left without a knee joint or with a painful and short leg as a result.
Activities To Avoid
Once you have your new knee replacement it is up to you to take care of it. Although the new knee replacement may feel much like a normal knee, it is not. It is much like the bearings in a car and it can wear out if too much force is applied to it. Avoiding excessive and undue stresses on the new knee will give it the best chance of having a long life.
Your knee replacement should feel very good and it can be tempting to return to all the activities you have missed out on because of your knee condition. However, the knee replacement is not designed for high impact activities. The longevity of your knee replacement is very dependant on how you treat it.
If the knee is abused it may wear out more quickly than expected. You should definitely avoid running or jogging, contact sports and high impact aerobics. You should try to avoid vigorous walking, hiking, skiing, competitive tennis and repetitive lifting exceeding 20kgs. The knee replacement is not designed for manual labour.
How long will your knee replacement last?
There is about a 1% chance per year that you will require a revision knee replacement. Knee revisions are much more difficult, they tend to have more complications and they have a less successful outcome than the original surgery. This is why it is so important to look after your new knee forever more. By looking after your new knee, you will be able to substantially improve the longevity of the knee and hopefully avoid the need for a revision knee replacement in the future.
There have been significant advances in knee replacement design, the materials that are used and the techniques used to put the knee replacement in. It is hoped that these will reduce the incidence of complications from the surgery, increase the longevity of the knee replacement and improve the performance of the knee replacement.
Commonly Asked Questions
What are the risks of surgery?
The risks of Knee Replacement Surgery can be thought of as general risks of the procedure and local risks to the knee and leg:
General Risks
These events are very rare
- Death is possible from the procedure
- There is a risk of having a problem with the heart such as a heart attack, heart failure or arrhythmia
- There is a risk of having a stroke These events are more common
- Clots in the legs may occur with pain and swelling of the legs. Rarely parts of the clots can break off and travel to the lungs. This can be fatal but everything possible is done to avoid this from happening.
- Small areas of the lungs can collapse following surgery that may cause infection in the lungs requiring antibiotics and physiotherapy.
- Bladder and prostate problems can be exacerbated by your surgery. A catheter is routinely placed in your bladder at the time of surgery to avoid this. This will be removed once you are comfortable and mobile.
The bowel may become paralysed after surgery. This may result in pain, bloating, nausea and vomiting for a time. Local Risks Infection after knee replacement. This can occur at any time. Therefore it is very important to be vigilant for the risk of infection. Infection often requires further difficult surgery that may result in revision knee replacement. A revision knee replacement is sometimes not possible and the knee needs to be fused or surgically stiffened. The knee is fused straight and it cannot bend at all; this is permanent. Sometimes the infection cannot be eradicated even with further surgery.
Extremely rarely amputation becomes necessary to eradicate infection.
- The knee may be stiff and or painful following the surgery. Sometimes the cause of this cannot be identified.
- A small proportion of patients will need to return to the operating theatre within three months to have a manipulation to help the knee bend. The patient then needs to stay in hospital for a number of days to continue physical therapy to ensure the knee continues to bend.
- The nerves about the knee joint can be injured at the time of surgery. This can result in pain or weakness. It can result in permanent disability. The most common nerve affected is the nerve that supplies the muscles to the top of the foot. Damage here can result in a foot drop.
- Rarely the limb can become painful, swollen, red and stiff with abnormal sensation, even following a well-performed knee replacement. This is due to an abnormality in the pain system and it can be very difficult to treat.
- The new knee joint itself may loosen and/or wear over time. This can result in pain and instability over time. The femoral component, the tibial component, the plastic bearing or the patella may fail individually or in combination. This may require revision surgery in the future. Sometimes this can result in bone loss about the knee joint which can lead to fracture of the femur or tibia in future years. A number of steps are taken to reduce the risks of this.
- There is a risk that the new knee may fail within the first five years. This will require further surgery.
- Occasionally the bone of the femur or tibia may break at the time of surgery. This is often recognised at the time and can be corrected during the knee replacement. This may mean you are not able to walk on the leg for a period of time following the surgery. Rarely you may need further surgery to treat the fracture.
- The wound may not heal properly and can become red, thickened and painful. Steps are taken to avoid this.
- Possible bleeding into the wound after surgery. This may become painful and require surgical drainage, or become infected and require antibiotics.
- There is a risk that the leg may have to be amputated due to poor blood supply or infection.
- There is an increased risk of complications in obese people of wound infection, heart and lung complications and blood clots.
- There is an increased risk of complications in patients with diabetes.
- There is an increased risk of complications in smokers.
- There is an increased risk of complications in patients with multiple medical problems.
- There is an increased risk of complications in the very elderly and infirm.
