Introduction
The following information is a guide to your upcoming surgery. It describes what is likely to happen at your upcoming surgery. This is a guide only and there may be some individual variation depending on your individual circumstances. Dr Lawrie will discuss these with you. Please become familiar with this guide and discuss any aspects you wish to with your surgeon, anaesthetist and/or nursing staff.
Carpal Tunnel Release is typically performed as a day procedure. You will be admitted and discharged on the day of surgery unless this is impractical or there are medical circumstances which preclude this. You must have a responsible adult to accompany you home and be with you overnight.
What is Carpal Tunnel Syndrome?
Carpal Tunnel Syndrome is compression of the Median Nerve at the wrist. The bones of the wrist (the carpus) form a C-shaped concavity (or tunnel) open at the front of the wrist. Through this travel the flexor tendons to the fingers and thumb and the Median Nerve. A thick ligament (the transverse carpal ligament) sits across the wrist bones forming the roof of the tunnel. When the pressure builds up in the carpal tunnel the Median Nerve is compressed and starts to dysfunction.
The Median Nerve typically supplies sensation to the Thumb, Index, Middle and half of the Ring fingers. It also supplies the small muscles which help with fine movement of the thumb. Typically when the Median Nerve is compressed pain is felt in the thumb to ring fingers. However the pain of Carpal Tunnel Syndrome can be quite variable, it can be felt in the fingers, wrist, forearm and even at times up to the shoulder.
As the nerve becomes more compressed numbness becomes more of a problem. The numbness also can be quite variable but is typically in the front of the fingers supplied by the median nerve. As the nerve becomes more compressed the muscles supplied by the nerve become affected. Weakness in the thumb and wasting of these muscles becomes evident.
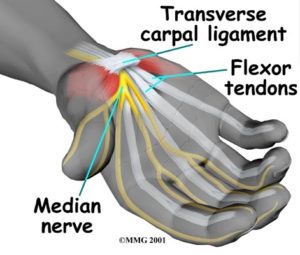
Carpal Tunnel Syndrome occurs because the pressure in the carpal tunnel has increased over time. At the time of surgery we commonly find that the transverse ligament has thickened up and the lining of the flexor tendons has thickened both of which reduce the space for the Median Nerve which gets compressed which affects the nerve’s function. Activities which reduce the volume of the carpal tunnel often produce the symptoms of Carpal Tunnel Syndrome; Pain or aching, numbness and weakness. It is very common for people to sleep with their wrists in a flexed position which is why it is common to wake at night with Carpal Tunnel Syndrome. This also explains why it is commonly felt while driving a vehicle.
The exact cause of Carpal Tunnel Syndrome is poorly understood. It is commonly exacerbated by situations in the workplace. People with Carpal Tunnel Syndrome often have other conditions of the hand such as trigger finger and DeQuervain’s disease which are due to the same process of thickening of the lining of the tendons of the hand (tenosynovitis). Osteoarthritis of the thumb is also common in patients with Carpal Tunnel Syndrome. Treatment of Carpal Tunnel Syndrome involves relieving the pressure on the Median Nerve. The first step is to ensure the diagnosis is correct. This is done by a thorough consultation with your surgeon involving a complete history and examination to exclude other causes of your symptoms.
Nerve Conduction Studies performed by a neurologist will be used to confirm the diagnosis (as the symptoms are quite variable) and to give an idea of the severity of the compression on the Median Nerve. Sometimes Carpal Tunnel Syndrome can settle without an operation especially if the cause can be identified and is temporary. Anti-inflammatory medications, night splints to avoid wrist flexion and occasionally injections of cortisone can be successful. Carpal Tunnel Syndrome in pregnancy is a common situation where the symptoms are temporary and can settle without an operation.
If the symptoms of Carpal Tunnel Syndrome are not settling and pain and disability are severe then an operation to release the pressure is the treatment of choice. This can be done through an endoscopic (keyhole technique using one or two 1centimetre incisions) or an open technique (a three to five centimetre incision). Both techniques involve transecting the transverse carpal ligament which releases the compression of the Median Nerve. The endoscopic technique involves using a telescope passed through one or two small incisions in the palm and wrist and hooked up to a video monitor. The transverse ligament is incised from below using a special knife and viewing the surgery on the monitor. It has the advantages of less post-operative pain and disability. There may be an earlier return to full functional activities. The may be less pain related to the scar and less pain due to muscular pain from an open incision. It has the disadvantages of being a technically more difficult technique with a potentially higher complication rate.
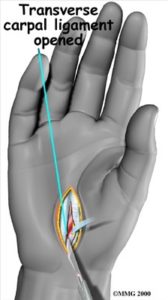
Some reports show a higher rate of damage to the tendons of the fingers and to the Median Nerve itself or to the muscular branch to the thumb. Damage to these structures can result in permanent pain and/or numbness and/or weakness. The endoscopic technique also has a higher risk of incomplete release of the transverse ligament and hence failure to relieve symptoms or recurrence of symptoms. The risk of complications can be reduced if the technique is only used when the hand has thin soft skin devoid of callosities. The open technique involves a three to five centimetre incision over the front of the wrist and releasing the transverse ligament from above under direct vision. It has the theoretical advantage of being able to see all the structures in the carpal tunnel and hence avoiding injury to them. However it is still possible to injure the flexor tendons and Median Nerve or its muscular branch to the thumb if there is abnormal anatomy.
The scar from the open technique can be quite sensitive but you will be instructed in techniques to reduce this. There is a higher incidence of pillar pain (pain at the base of the little finger or thumb) due to the muscles to these digits being incised during the incision. This usually settles over about six weeks but can take longer. It is generally understood that the open technique does have slightly more postoperative pain and disability but is probably a safer technique for the average patient and surgeon
Before Surgery
You should stop anti-inflammatory drugs at least five days prior to surgery as they can increase the chance of bleeding (e.g. Voltaren, Naprosyn, Nurofen, Brufen, Feldene, Naprosyn and Indocid. Celebrex and Mobic are not a problem). You may continue to take low dose aspirin (to prevent heart attack or stroke)
It is extremely important you have no cuts, scratches or sores on the involved limb at the time of surgery. If present these increase the chances of infection. If present your surgery should be postponed till all are well and truly healed. On the day of surgery a nurse will inspect your limb for lesions. The nurse will use clippers to remove long hair from the wrist (if present) and dress the wrist with an antiseptic solution.
Dr Lawrie will also inspect the limb and mark the appropriate limb to be operated on with an indelible marking pen. You should stop smoking prior to surgery. Smoking increases the risks associated with an anaesthetic and the risk of blood clots (DVT) following surgery.
Admission
You should not eat or drink 6 hours prior to surgery. You should bring with you;
- Personal effects (nightgown or pyjamas, slippers, dressing gown, toiletries) in case you are required to remain in hospital overnight.
- Any medication you are taking
- All relevant x-rays, scans and reports
- Medicare and private health fund membership cards
- This paperwork
Prior to going to the operating room, you will be taken to the Day Surgery Unit and you will;
- Have a shower with an antiseptic soap
- Be dressed in a theatre gown and disposable underwear
- Have the limb inspected and dressed with an antiseptic solution and sterile drape
The procedure
You will be taken into the operating room on a trolley by the nursing staff. The operation will take about fifteen minutes but you may spend up to one hour in the theatre complex by the time you wait in the pre-operative area, are prepared from your anaesthetic and then woken up in the recovery area.
The Anaesthetic
The operation can be performed under local anaesthetic only, local anaesthetic and sedation or a general anaesthetic. Dr Lawrie will discuss this with you prior to surgery. Commonly Carpal Tunnel Release is performed under local anaesthetic block. This involves injecting local anaesthetic with a very fine needle into the front of the wrist joint where an incision will be made.
The local anaesthetic stings as it is injected, however the area rapidly becomes numb ready for surgery. A tourniquet is applied to the upper arm to allow a bloodless operative field thereby facilitating surgery. This is inflated just before the surgery is commenced. It can be quite tight on your arm, and is only inflated for a short time.
A drip will be placed in the back of your other hand where anaesthetic medicines and antibiotics can be injected. For some patients a sedative will be injected into your drip by the anaesthetist which will send you to sleep during the procedure.
The Surgery
You will be placed on the operating table lying on your back. A well padded tourniquet will be applied to your upper arm and inflated to a safe level just prior to the commencement of surgery. You arm will be laid out to your side on the operating table. Your arm will be prepared with an antiseptic solution and sterile drapes will be placed around the arm and over your body. The drapes will be placed so as not to cover your face. You will not be able to see the surgery.
The theatre staff will talk to you through the surgery and music will be played to you all to help keep a calm and pleasant environment for your surgery to take place. A three to five centimetre incision is made on the front of the wrist joint in such a way as to avoid excessive scarring and damage to important nerves, blood vessels and tendons. The transverse carpal ligament is incised releasing the pressure on the Median Nerve.
Great care is taken to ensure the ligament is completely released (incomplete release of this ligament is one of the causes of recurrence of symptoms). The carpal tunnel is then inspected to exclude rare causes of the disease. The Median Nerve is inspected to ensure no injury has occurred through surgery and the degree of narrowing of the nerve can give and indication of the prognosis for recovery. The skin is then closed with a nylon suture and a firm dressing is applied. The tourniquet is deflated and you will be moved into the recovery area.
The Recovery
If you have had a general anaesthetic the anaesthetist will reverse the anaesthetic. You will wake up in the recovery room. The nurse will check your observations and movement in your fingers. Once you are sufficiently awake you will return to the Day Surgery Unit.
After Surgery
Dr Lawrie will see you before you go home and explain the operative findings to you. A copy of the operative report will be given to you and sent to your local doctor. For pain control you will have tablets available to take home with you (Panadiene forte/ Tramal/ Digesic). You may also be given an anti-inflammatory type medication.
You may resume any previous medications that you were receiving before surgery. If you have any allergies, these should be discussed prior to your discharge. Do not drive or use machinery after taking these medications. You can travel home in a car, but can not drive. If you are travelling more than 100km you should consider staying locally that night or overnight in hospital.
The night of surgery your wrist should be reasonably comfortable due to the local anaesthetic. This typically wears off after 12-18 hours. It is normal to experience some discomfort the following day as this wears off.
When You Get Home
The amount of post-operative discomfort can be quite variable. Many patients will be back to normal in two or three weeks. The wrist can be quite tender and painful for four to six weeks.
Typically you will need help with everyday activities such as dressing, preparing meals and driving. If you have both sides done at the same time then even simple activities such as toileting will need help. Return to work may take four to six weeks. The bulky bandage should remain on your wrist for three days to help with postoperative swelling. This compression dressing should be comfortable and absorb any leakage of fluid and/or blood.
Although the dressing may become moist or blood stained, this is not a cause for alarm. After three days the bandage can be removed and small primapore type dressings can be applied. It is very important that the surgical wound is kept clean and dry whilst it is healing. The wound is generally healed after 12 days. Sutures should be removed at day 10-14 post-operatively. Sometimes steri-strips need to be applied to the wound once the sutures are removed.
You may drive a vehicle when you can make a full fist with no discomfort and are not taking pain killers that may cause drowsiness. It is a good idea to consult with your insurance company about when you can return to driving. You will be seen for follow-up in Dr Lawrie’s rooms after the surgery. The timing of which will be decided on at the time of surgery. We will again discuss the findings at the time of surgery, what surgery was performed and what the future holds for your wrist.
Diet – You may resume your diet as tolerated but should avoid greasy foods for the first 24 hours. Bruising – Bruising may be considerable on the front of the wrist and extend down into the palm and up into the forearm. Experience has shown that the bruising and swelling resolve without difficulty within a few weeks.
Incisions – The surgical incision usually heals after about twelve days. The incision should be kept clean and dry until well and truly healed. Incisions over the front of the wrist and palm can be quite sensitive. This is due to the large number of small sensory nerve fibres present in the area. Once the sutures are removed massaging the wound twice a day with a water-based cream such as sorbelene or vitamin E cream can prevent a sensitive scar forming.
Physiotherapy – With all hand surgery the final result that you achieve is greatly dependent upon the amount of rehabilitative effort you make .The keys to your rehabilitation are elevation and early movement. The wrist should be elevated on two to three pillows at night and kept above the heart for the first five to seven days were possible. Avoid holding the wrist in a dependant position. The fingers should be mobilised from day one. Open and close the fingers one hundred times four times per day. Once the dressing is removed wrist exercises can be commenced. No heavy lifting should be performed for six weeks.
Results
Carpal Tunnel Release typically has very good results. Your recovery is dependant upon how long and how severe the compression of the median nerve has been. If you have any concomitant diseases such as diabetes or other nerve conditions then recovery may be affected. Smoking may also affect recovery Pain is generally relieved well from Carpal Tunnel Syndrome, but can be incomplete. Numbness or pins and needles has a more variable chance of recovery and tends to take longer. Weakness takes the longest time to recover and can be permanent. Nerve function can recover over a period of months to even years and is dependant on the patients’ age and medical condition.
Precautions
If you develop a fever above 39 degrees centigrade, unexpected pain, redness or swelling in your wrist please contact our office or the hospital. Return appointment Please call our office on 5444 3511 to make your first follow up appointment for approximately 2 to 4 days following your surgery If you have a problem such as vomiting the same night of your surgery, you should contact the nursing supervisor/ senior nurse on the surgical ward at the hospital you had your surgery at.
Commonly asked questions
Will my surgery be successful?
Carpal Tunnel surgery has a high success rate with a very low complication rate. However patients often have a painful incision for about six weeks. Pain responds favourably however numbness and weakness may not respond as well.
Will I need further surgery?
It is uncommon to need further surgery but Carpal Tunnel Syndrome can recur. This is probably slightly more common with the endoscopic technique. It is not uncommon to need surgery for trigger finger or DeQuervain’s disease in the future. When can I start swimming? Swimming is an excellent exercise and I would strongly encourage swimming following surgery. Once the wounds are well healed, after about 2-3 weeks, then a swimming programme to complement your physiotherapy is a good idea.
When can I return to work?
This varies from individual to individual. Often at two weeks one can resume light duties but this can often take six weeks. When can I return to sport? Once pain and swelling has settled and you can form a full and supple fist with full power, then a return to sport can be instituted. This may take 1-2 months.
Download