What is Dupuytren’s Contracture?
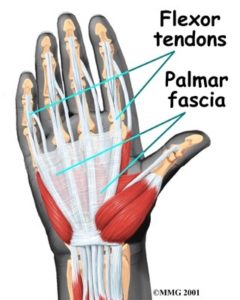
Dupuytren’s contracture is caused by a thickening of normal fibrous tissue bands which run from the palm into the fingers. The ring and little fingers are those most commonly involved initially. The condition produces lumps in the palm and dimpling of the skin because it is tethered to these fibrous bands. Finally the fingers are contracted towards the palm and cannot be straightened. In most cases, both hands are involved.
Pain is sometimes an early feature, when lumps are forming in the palm. After this, pain is rarely a problem. Contracture of the fingers leads to difficulty using the hand. Severe deformity leads to problems with the skin in the palm which cannot be washed and dried normally. It is the knuckle joints that usually contract first, followed by the finger joints. It usually worsens quite slowly, but more rapidly in young men.
How does Dupuytren’s Contracture occur?
The trigger that starts this disease off is unknown, although injury seems to be a factor in some people. The fibrous tissue which develops is very much like scar tissue. It binds the skin to the coverings of the finger tendons (sinews) and then shrinks and contracts to produce the deformity.
Why does Dupuytren’s Contracture occur?
The problem is more common in males and tends to run in families. It is more common in those over 60 years of age, and is more often found in people with epilepsy, cirrhosis of the liver, or diabetes. There is no definite relationship to occupation.
Treatment Involved for Dupuytren’s Contracture
In mild, slowly progressive cases, no treatment is necessary. Treatment should be sought before severe contracture occurs, and particularly if deformity increases rapidly. Operation is usually carried out once the knuckle joints are contracted to a disabling degree or the finger joints are affected in any way at all. If finger joints are allowed to become very contracted, permanent joint stiffness is likely, despite surgery. Surgery may be carried out under either local or general anaesthesia. A variety of different skin incisions may be used. The thickened contracted tissue is removed, releasing the joint. In very severe or recurrent cases, skin grafts may be required. When the little finger is completely contracted into the palm, surgery rarely achieves a full release.
In this situation amputation may be recommended. Simple division of a fibrous cord in the palm is very rarely used alone to release isolated contracture of a knuckle joint. Incisions in the fingers are always stitched. Those in the palm are also usually closed, but sometimes in severe contractures may be left open to heal. A protective plaster of Paris splint is sometimes used. During the first 48 hours the hand is elevated to prevent swelling and to decrease pain.
The majority of patients stay in hospital overnight and are able to leave the following day. The keys to a good result in Dupuytrens disease is complete removal of the diseased tissue at the time of surgery, avoidance of scarring with special releases made in the skin incision and very importantly early and regular hand therapy. Patients with severe contracture may need to wear a resting splint for several weeks after the surgery to limit scarring and recurrence of the contracture.
During Treatment for Dupuytren’s Contracture
The formation of a bruise underlying the wound is the most troublesome complication. Infection often follows this problem and prevents early movement, leading to stiffness. Severe pain in the immediate post-operative period is usually due to bleeding or bruising. When this occurs soon after operation, the surgeon may decide to release the blood clot.
In extensive or recurrent cases, areas of the skin can die because their blood supply is lost. Small areas of skin loss are usually not a problem. Skin grafting is sometimes necessary for larger areas. The nerves to the fingertip can be damaged during surgery causing numbness and pins and needles in the fingertip. If the nerve has only been stretched, it usually recovers. However, especially in re-operated cases, the nerves are much more likely to be permanently damaged.
After Treatment for Dupuytren’s Contracture
You will need hand exercises which will be supervised by a Hand therapist following discharge from hospital. If one of your fingers was very contracted prior to surgery, then splints to keep the fingers straight are usually used. This type of splint is worn continuously initially and then at night to maintain the corrected position. It may continue to be worn at night for several months.
In general, full release of the knuckle joint is achieved and maintained. The final result in finger joints depends on the degree of contracture present before operation. If this is severe, it may amount to a 50 to 75% correction only. It is important to keep the scars and skin supple usually with hand cream(your hand therapist will instruct you on this). Return to work depends on occupation and whether the dominant hand was operated upon.
In general, clerical work can be resumed after 2 to 4 weeks, and manual work rather later at 4 to 6 weeks. Regular stretching helps to keep the fingers straight. The condition can come back after operation or may extend from the original area. This is more likely if the initial contracture developed rapidly in a young person. The need for operation following recurrence is assessed in a similar way to new cases. Skin grafting is more likely to be required following recurrence. After operation, full movement of the fingers must be kept up. Increasing
If Dupuytren’s Contracture is Left Untreated
If not treated, the disease may develop so slowly that no treatment is necessary. It may, however, produce marked contracture of the fingers. The fingertips then become fixed in the palm, limiting function and causing skin problems. If left too long and the contracture becomes too severe than the only surgical solution may be amputation especially when cleaning the hand and finger become difficult.
Download