Introduction
The following information is a guide to your upcoming surgery. It describes what is likely to happen at your upcoming surgery. This is a guide only and there may be some variations depending on your individual circumstances. Dr Lawrie will discuss these with you.
Please become familiar with this guide and discuss any aspects you wish to with your surgeon, anaesthetist and/or nursing staff. Knee arthroscopy is typically performed as a day procedure. You will be admitted and discharged on the day of surgery unless this is impractical or if there are medical circumstances which preclude this. You must have a responsible adult to accompany you home and be with you overnight.
How The Normal Knee Works
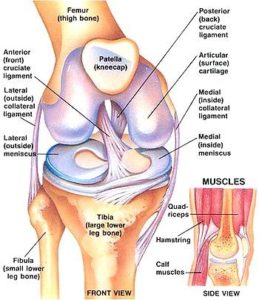 The knee is the largest joint in the body and one of the most easily injured. It works as a complex rotating hinge. It is made up of the lower thigh bone (the femur) the upper end of the shin bone (the tibia) and the kneecap (the patella) which lies at the end of the femur. There are 4 major ligaments which control the movement and stability of the knee joint;
The knee is the largest joint in the body and one of the most easily injured. It works as a complex rotating hinge. It is made up of the lower thigh bone (the femur) the upper end of the shin bone (the tibia) and the kneecap (the patella) which lies at the end of the femur. There are 4 major ligaments which control the movement and stability of the knee joint;
The medial ligament is on the inside of the knee.
The lateral ligament and posterolateral corner is on the outside of the knee. These two ligaments control mainly side to side movement.
The anterior cruciate ligament and the posterior cruciate ligament sit one behind the other on the inside of the knee and these are very important ligaments for stability from front to back and rotation. The strong thigh and calf muscles add to strength and stability and also control the movement of the kneecap. The ends of the bones are covered in specialised cartilage called hyaline or articular cartilage which allows for very smooth friction-free movement about the knee. This is the surface that is damaged in osteoarthritis or wear and tear arthritis or inflammatory conditions such as rheumatoid arthritis. It can also be damaged due to trauma and sports injuries. Sitting on top of the surface of the tibia are two c-shaped cartilages called the meniscus. The meniscus can be thought of as the shock absorber in the knee. They absorb much of the forces that pass through the knee and dampen the shock that is applied to the articular cartilage. They also add some stability to the knee as well as nutrition to the joint surface. The knee joint is surrounded by a thin connective tissue layer called synovium that secretes lubricating fluid which reduced the friction to nearly zero in a healthy knee but when this is inflamed it can cause considerable pain and swelling.
The Surgery
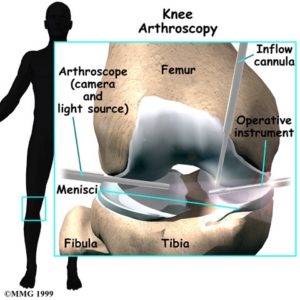
A knee arthroscopy is a common operative procedure. It involves placing a telescope into the knee through a small keyhole incision. The telescope is attached to a video monitor which allows a thorough inspection of the knee joint. Fine instruments can be placed through one or two small separate incisions within the knee to treat various conditions in the knee. The arthroscopy can be used both to diagnose conditions as well to treat many problems within the knee. The most common reason to perform a knee arthroscopy is to treat a torn meniscal cartilage.
 The meniscus can tear for two reasons. Usually it will tear due to ageing of the meniscus or if it has a poor blood supply and a poor ability to heal. Typically a person will bend their knee 3 million times a year and the meniscus is loaded throughout the day. The meniscus typically suffers multiple minor insults over its lifetime and eventually it fatigues and splits to form a full tear within its body. This usually results in mechanical pain and swelling in the knee and sometimes locking of the knee.
The meniscus can tear for two reasons. Usually it will tear due to ageing of the meniscus or if it has a poor blood supply and a poor ability to heal. Typically a person will bend their knee 3 million times a year and the meniscus is loaded throughout the day. The meniscus typically suffers multiple minor insults over its lifetime and eventually it fatigues and splits to form a full tear within its body. This usually results in mechanical pain and swelling in the knee and sometimes locking of the knee.
In this situation an arthroscopy is used to remove only the torn piece of cartilage, leaving the remaining untorn cartilage in the knee to hopefully continue its function as a shock absorber. Recovery from this surgery is quite rapid. You will be able to walk on the knee the following day. Quite rarely some people need crutches for pain relief but the knee typically settles down very quickly and returns to normal in around 2-4 weeks.
Prior to arthroscopic surgery an MRI scan can be very valuable in evaluating the knee injury and to allow planning of the surgery. The meniscus can also tear due to trauma or a sporting injury. In this situation, the meniscus was normal before it tore but an extreme injury to the knee can result in a tear of the meniscal body. This is often associated with a major ligament tear. Typically this is in the young sporting patient and the most common situation is when a patient tears their anterior cruciate ligament and their medial meniscus.
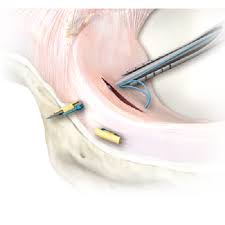
In an acute tear it can be possible to repair that meniscus and there are a number of devices that can be used to sew this up and encourage healing of that meniscus. If a meniscal repair is possible then the knee is in a much better situation because once that meniscus is healed it should return to its full shock absorber function.
The difference in the surgery here is that it is much more complicated surgery and the meniscus needs to be protected following the surgery. This typically involves being placed in a brace for 6 weeks and not weight bearing through that knee for 6 weeks to allow that meniscus to heal. Typically it takes 3-6 months for the meniscus to completely heal and often this surgery is accompanied by ligament reconstruction surgery as well.
Microfracture
As the knee ages the more likely there is to be some wear and tear damage to the articular surface as well as a tear to the meniscus. An MRI scan is very good at predicting the presence of a meniscal tear but not as good at predicting damage to the articular surface. If at the time of an arthroscopy, typically when treating a torn meniscus, it is found that there is an area of the articular cartilage that is particularly damaged and worn almost or down to bone then a microfracture technique can be performed arthroscopically to encourage new cartilage to form.
This technique involves performing multiple punctures through the base of the defect into healthy bone to encourage new cartilage growth. This can be a very useful technique to slowdown the wear and tear changes in the knee and this is a very simple procedure and only adds a few minutes to the arthroscopy. It does not cause any extra pain but it is very important to protect the knee following this surgery.
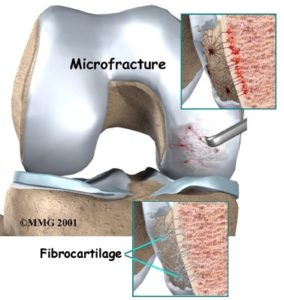
Typically the patient is not allowed to weight bear through that knee for a period of 6 weeks following the surgery to allow the new cartilage to heal. A further six weeks avoiding heavy lifting, twisting and rotational loads will allow the healing fibrocartilage to mature. Taking glucosamine and chondroitin sulfate may help with the healing process.
Many other conditions in the knee can be treated arthroscopically as well. Loose fragments of bone or cartilage can be removed and damaged joint surfaces or softening of the articular cartilage can be treated as well as inflammation of the synovium membrane, such as with rheumatoid arthritis or gouty arthritis. Infection of the knee and abnormal alignment or instability of the kneecap and diagnosis and reconstruction of the ligaments about the knee can also be done arthroscopically.
Before Surgery
You should stop anti-inflammatory drugs at least five days prior to surgery as they can increase the chance of bleeding (e.g. Voltaren, Naprosyn, Nurofen, Brufen, Feldene, Naprosyn and Indocid. Celebrex and Mobic are not a problem). You may continue to take low dose aspirin (to prevent heart attack or stroke) It is extremely important you have no cuts, scratches or sores on your leg at the time of surgery. If present these increase the chances of infection. If present your surgery will be postponed till all are well and truly healed. On the day of surgery a nurse will inspect your leg for lesions. The nurse will use clippers to remove long hair from the knee and dress the knee with an antiseptic solution. Dr Lawrie will also inspect the leg and mark the appropriate leg to be operated on with an indelible marking pen.
You should stop smoking prior to surgery. Smoking increases the risks associated with an anaesthetic and the risk of blood clots (DVT) following surgery.
Admission
You should not eat or drink 6 hours prior to surgery. You should bring with you:
- Personal effects (nightgown or pyjamas, slippers, dressing gown, toiletries) in case you are required to remain in hospital overnight.
- Any medication you are taking
- All relevant x-rays, scans and reports
- Medicare and private health fund membership cards
- This paperwork Prior to going to the operating room, you will be taken to the Day Surgery Unit and you will:
- Have a shower with an antiseptic soap
- Be dressed in a theatre gown and disposable underwear
- Have the limb inspected and dressed with an antiseptic solution and sterile drape If you wish Dr Lawrie to speak to a family member after the operation please notify the nursing staff with contact details.
The Procedure
You will be taken into the operating room on a trolley by the nursing staff. The operation will take about thirty minutes but you may spend up to one and a half hours in the theatre complex by the time you wait in the pre-operative area, are prepared from your anaesthetic and then woken up in the recovery area.
The Anaesthetic
The anaesthetist will give you a general anaesthetic and will discuss this with you prior to the operation. A drip will be placed in the back of your hand where anaesthetic medicines and antibiotics can be injected. You will be asked to breathe into an oxygen mask and the drugs to make you fall asleep will be injected through that drip. You will be asleep and not aware of anything further until the operation is over and you wake up in the recovery area. It is not uncommon to have some amnesia prior to or immediately after the surgery due to the anaesthetic drugs.
The Surgery
You will be placed on the operating table lying on your back. A well padded tourniquet will be applied to your thigh and inflated to a safe level just prior to the commencement of surgery. The tourniquet prevents bleeding into the knee and so allows the surgeon to see and perform the surgery more easily. Two to four small one centimetre incisions placed about the knee will be used to gain access to the knee. Through one of the incisions (or portals) the arthroscope will be introduced. The arthroscope is like a telescope and is attached to a light source and a video camera.
The video camera is attached to a monitor which allows images of your knee to be projected onto the screen. The arthroscope is also attached to a fluid source (salty water) which constantly flows through the knee. This allows the arthroscope to be manoeuvred through the knee and gives a good image on the screen. It also allows any debris or inflammatory chemicals produced within the knee which are causing you pain to be washed from the knee.
All aspects of the knee joint are inspected in a stepwise manner so as to minimalise the risk of missing pathology. Through a second portal fine instruments are introduced which are used to correct the injury or disease within your knee. These instruments include scissors and electronic and manual tissue resecting devices.
Suturing devices can also be used. Usually no further incisions are necessary. On occasion if certain suturing techniques are used or a large piece of tissue needs to be removed from the knee a larger incision may be necessary. Procedures such as knee ligament reconstruction require more and/or somewhat larger incisions to obtain a graft and accurately place the graft within the knee. At the end of the procedure your knee will be injected with a combination of local anaesthetic and morphine.
Steri-strip (bandaid like dressings) or sutures will be used to close the wounds. Occasionally a drain may be placed in your knee at the end of the procedure to prevent a large haematoma (bruise) forming. This will be removed prior to discharge. A sterile dressing will be applied to your knee. A large bandage will be placed around your knee to prevent bleeding and swelling.
The Recovery
The Anaesthetist will reverse the anaesthetic and you will wake up in the recovery room. The nurse will check your observations and movement in your feet. Once you are sufficiently awake you will return to the Day Surgery Unit.
After Surgery Dr Lawrie will see you before you go home and explain the operative findings to you. A copy of the operative report will be given to you and sent to your local doctor. Once you are well and truly awake you will be visited by the physiotherapist who will instruct you on a series of exercises to get the best result from your operation. This will be targeted at strengthening specific muscle groups so as to protect the knee from damage in the early post-operative stages and to get the knee on its way to moving normally again.
Only very rarely do patients need to use crutches at least for the first few days until they are steady on their feet. Most patients are allowed to put all their weight through the limb on the day of surgery. For pain control you will have tablets available to take home with you (Panadiene forte/ Tramal/ Digesic/Endone). You may also be given an anti-inflammatory type medication.
You may resume any previous medications that you were receiving before surgery. If you have any allergies, these should be discussed prior to your discharge. Do not drive or use machinery after taking these medications. You can travel home in a car, but can not drive. If you are travelling more than 100km you should consider staying locally that night or overnight in hospital.
The night of surgery your knee should be reasonably comfortable due to the local anaesthetic and morphine within the knee. This typically wears off after 12-18 hours. It is normal to experience some discomfort the following day as this wears off. When You Get Home The amount of post-operative discomfort can be quite variable and is dependant on the type and amount of surgery that was performed.
It is quite normal for the knee to be painful and stiff for the first two weeks. It often takes up to six weeks before the knee is feeling right and you can return to full activities such as sport or manual labour. On occasion this can be longer. If you experience severe pain or swelling or have any worries contact Dr Lawrie or and/or your local doctor. The bulky bandage should remain on your knee for 3-4 days to help with postoperative swelling. This compression dressing should be comfortable and absorb any leakage of fluid and/or blood.
Although the dressing may become moist or blood stained, this is not a cause for alarm. After 3-4 days the bandage can be removed, the dressings over the wounds should remain in place for 10-14 days. When the bandage is removed the knee may continue to swell for days to sometimes weeks after. Using a neoprene knee sleeve or tubigrip bandage is very useful if swelling continues. The knee sleeve should be firm but not too tight or uncomfortable so as to cause pain. The knee sleeve should be used intermittently so as not cause undue sweating and skin irritation or significant indentation of the skin. Regular ice can be very useful to treat swelling.
It is very important that the surgical wounds are kept clean and dry whilst they are healing. The wounds are generally healed after 12 days. If sutures are present these should be removed at day 12-14 post-operatively. Steri-strips should be allowed to fall off on their own after day 10. You may drive a vehicle when you can walk comfortably without crutches and when you are not taking pain killers that may cause drowsiness.
It is a good idea to consult with your insurance company about when you can return to driving. You will be seen for follow-up in Dr Lawrie’s rooms after the surgery and the timing of this will be decided at the time of surgery. We will then discuss the findings at the time of surgery, what surgery was performed and what the future holds for your knee.
Diet
You may resume your diet as tolerated but you should avoid greasy foods for the first 24 hours. Bruising – Bruising may be considerable on the back and outer side of the knee and also the thigh and calf. There also may be some bulging along the outer side of the kneecap. Experience has shown that the bruising and swelling resolve without difficulty within a few weeks.
Incisions
The small surgical incisions are usually left open to allow drainage of the fluid used during surgery, but may on occasion be stitched. The small points of entry may be sore and may develop bruising during the first few days after surgery. This bruising around the wounds will eventually disappear and does not require any special care.
Physiotherapy
Unless you have a chronic joint condition or unless an arthroscopy was done for diagnosis only; the arthroscopic surgery should have improved the condition of your joint. Occasionally during an arthroscopy, an injury or disease will be discovered that cannot be treated adequately with arthroscopy alone. In order to achieve optimal recovery, an extensive amount of work with the supervision of a physiotherapist is necessary. The final result that you achieve is greatly dependent upon the amount of rehabilitative effort you make. This will be discussed at the time of your first follow-up visit to the office. Physiotherapy should start within the first week after surgery.
Activity
Crutches are usually not necessary for walking after arthroscopy (unless microfracture of a meniscal repair is performed) but they may be necessary for comfort. You may place weight upon your surgical leg when comfortable. Active motion and tightening of the quadriceps muscles (muscles on the front of the thigh) should start the day of surgery. A twice daily exercise session for 15 minutes which would include motion and muscle contractions should be continued for at least 3 weeks at home following the surgery. Jogging or running should be deferred until your muscles have restrengthened. If a severe arthritic condition exists within the knee, then crutches will be necessary, and additional modifications of activity will be recommended. If deep stitches were placed within the joint or the kneecap, a brace will be necessary to limit knee motion for several weeks.
What Exercises To Do
Building up the muscles that support your knee and improving joint mobility is the best way to speed up your recovery. The following exercises are recommended and are to be done lying flat on your back.
QUADRICEPS SETS Tighten your front thigh muscles (quadriceps), pressing your knee toward the floor. Hold for 5 seconds then relax.
STRAIGHT LEG RAISES Lift your leg 30cms, keeping your knee straight. Hold for 5 seconds, then lower your leg slowly back to the ground.
HEEL SLIDES Bend your knee and slide your heel toward your hip as far as you can. Hold for 5 seconds and then slide back down until your knee touches the floor.
RELIEVING PAIN Do not dangle your leg for long periods of time. You must elevate your knee above heart level to reduce swelling and pain. Ice and rest can also help. During the first few days after bandage removal, apply ice to your knee for 20 minutes, 3 times a day.
Depending on your needs, a physiotherapist can design a personalised exercise program to help improve your muscle strength and joint function. Results Preliminary reports, as well as our experience, have shown that arthroscopic surgery produces results equal to if not better than surgery performed by open methods.
The benefits of arthroscopic surgery are less discomfort, less risk and less scarring for the patient. We frequently remind patients that although the external incisions are small, they have still had an operative procedure inside their joint. Experience has shown that internal healing takes several weeks. In fact, complete healing to mature tissue following arthroscopic surgery may take 3 months or more and at that time most patients will have major improvement in joint function.
Precautions
If you develop a fever above 39 degrees centigrade, unexpected pain, redness or swelling in your legs, please contact our office or the hospital. Please call our office on 5493 3994 to make your first follow up appointment following your surgery. If you have a problem such as vomiting on the same night of your surgery, you should contact the nursing supervisor or senior nurse on the surgical ward at the hospital where you had your surgery.
Commonly Asked Questions
Will my surgery be successful?
Depending on the reason for surgery, knee arthroscopy typically has a high success rate. Debridement (cleanup/washout) operation for osteoarthritis (wear and tear disease) may not be as successful as for acute injuries. However if one meets certain criteria then a washout can be expected to have a high success rate.
Will I need further surgery?
Arthroscopic surgery of the knee is good for removing/correcting mechanical problems in the knee. However, it may not address this problem. If you have wear and tear arthritis of the knee an arthroscopy can give good short to medium term results but in the long term you made need further surgery. One may think of arthroscopy as a temporising measure in these situations.
When can I start swimming?
Swimming is an excellent exercise and I would strongly encourage swimming following surgery. Once the wounds are well healed, after about 2-3 weeks, then a swimming programme to complement your physiotherapy is a good idea.
When can I return to work?
If you work in a sedentary job then most patients return to work the week following surgery. Manual labour can be resumed once pain and swelling is settled and when you are walking normally and have good quadriceps power. Usually this is after 1-2 weeks but may be longer. It is important that the swelling is settling before returning to heavy activity. It is normal to fell some discomfort on return to work. This usually settles relatively quickly as the knee gets used to the work environment again.
You may need to ice the knee at the end of the day, a knee sleeve at work can be useful. Some patients will find a short course of anti-inflammatory medications helpful during the early stages of return to work.
When can I return to sport?
This will depend on the type of surgery that was performed and, like the work situation, once pain and swelling is settled, you are walking (and running) normally and have good quadriceps power. Then a return to sport can be instituted. This may take 1-2 months.
Risk Of Complications
Generally speaking the risk of complications following arthroscopic surgery is very low. It is usually a very simple straight forward procedure taking very little time with a rapid recovery. As with any surgery complications are possible, general medical problems such as chest infection, angina, heart attacks, strokes, major blood clots and even death are possible from any surgery but major problems such as these are extremely uncommon after arthroscopy of the knee. However if you suffer from any major medical problems then the risk of complications is increased.
Deep infection of the knee joint is also very uncommon being in the order of 0.1% to even 0.01% in some reports. However the operation still needs to be respected and risks can not be taken before or after the surgery with respect to infection. Blood clots or DVT (deep vein thrombosis) can occur after any surgery. These once again are very uncommon after arthroscopy but need to be dealt with if they occur.
Any swelling about the calf or undue pain remote to the operative site needs to be dealt with urgently in case a DVT is developing. If you have a pre-disposition to blood clots ensure you have made Dr Lawrie, your anaesthetist and your GP aware of this prior to your surgery.
Osteonecrosis is a condition where a sudden loss of blood supply to the bone occurs. It can lead to a rapid form of arthritis. It is not uncommon in the women in their 6o’s but can happen to anyone at any age. It is extremely rarely seen after arthroscopy, it is unclear whether than is any cause and affect from the arthroscopy at this point in time. However it may be due to impact on the knee to soon after surgery. This condition is typically seen in the first six weeks following surgery as the knee needs to time to adapt to the mechanical changes following surgery. In older knees it appears important to avoid impact on the knee in the first six weeks. Long walks should be avoided as well as manual labour during this time.
Download