Which Hip Replacement Best Suits My Hip?
INTRODUCTION
The following information is a guide to your upcoming surgery. There are many options available when choosing an appropriate hip replacement for your hip. This document is to help explain the various techniques and implants available to you. It describes mini-invasive surgery (keyhole surgery), cemented vs uncemented hip replacement and the various alternative bearing surfaces available. It also discusses surface replacement arthroplasty. This document should be read in conjunction with Dr Lawrie’s Patient Pathway on Total Hip Replacement.
Hip Replacement Surgery
The hip joint is a ball and socket joint. Arthritis of the joint involves wear of the gliding surfaces of the ball and socket i.e. the articular cartilage. This results in pain and stiffness of the hip. As time goes on, soft tissues contract about the hip resulting in deformity, bone loss becomes more apparent and contributes to deformity and shortening of the limb. Hip Replacement surgery involves replacing the ball and socket with a pin down the centre of the femur with a ball attached as the head and replacing the socket with a hemispherical socket fixed to the pelvis. The aim is to give a relatively pain-free hip joint that is stable and has corrected the deformities present so the patient can return to a comfortable life, free of pain.
Mini-Invasive Surgery
MIS surgery describes the surgical approach to the Hip Replacement i.e. that is the way the surgeon operates on your tissues to get to the hip replacement. The actual components placed in the hip replacement are the same whether MIS is used or a traditional approach is used. Mini-Invasive Surgery (MIS) or keyhole surgery for hip replacement offers a less invasive alternative approach to hip replacement surgery. MIS surgery involves inserting the hip replacement through a much smaller incision (around 8-12cm) than the previous incisions of 20-30cm. The real difference in the MIS approach is not the size or look of the skin incision but what goes on underneath the skin that is important. MIS is a new approach to Hip Replacement surgery and hence there are no long-term studies on the outcomes of this surgery. Early studies are encouraging and show advantages over the traditional approaches.
About 5-10 years ago MIS surgery became possible. Some surgeons were pushing the envelope with how small a skin incision could be made to put in a hip replacement, some surgeons were describing as little as a 6cm incision. What has made this possible is the huge improvements in instrumentation now available to perform hip replacement surgery. The key to long term outcomes of hip replacement surgery is accurate placement of the components at the time of surgery. No matter what the size of the incision the surgeon must be able to see what they are doing and view the relevant landmarks/anatomy to gain as accurate placement as possible with the ultimate hip components.
Most surgeons realise that ultra-small incisions e.g. 6cm don’t allow an adequate view to achieve this in most situations. What we have also learnt from MIS however is the surgeon doesn’t have to release (or cut) as much of the soft tissues around the hip as we did previously in traditional large incision hip replacement. So what we now have is probably best described as small incision surgery. Typically the skin incision starts off at 10cm and is lengthened as necessary often 1 or 2cm if a better view is needed. Under the skin which is far more important than the length of the skin incision only those tissues necessary to exposure the joint itself are released. In some circumstances wide exposure is needed for severe deformity or dealing with other issues which may arise so it is important that the approach can be lengthened if necessary.
The advantages of these approaches over the traditional approaches are:
- Smaller more cosmetic incision
- Less tissue trauma
- Less blood loss
- Less post-operative pain
- Quicker post-operative recovery
- A more stable hip
- Lower complication rate
- Less scarring therefore easier revision surgery
- Less operative time
- Standard components are used
Type of incision
Two incision technique developed by Zimmer. This technique was heavily marketed by the company about 10yrs ago. Subsequent studies reveal it to be substandard with very high complication rates and has now been abandoned.
Posterior approach
This is the most common approach in Australia and perhaps the world. The incision is placed along the buttock and the muscles behind the hip are split to allow access to the hip joint. It can be performed through small and MIS techniques but can be extended to allow access to all areas of the hip if needed. When comparing approaches to the hip the risk of dislocation is slightly higher than an anterior approach, but this can now be minimised by improvements in components, a strong repair of the hip capsule at the end of the case and releasing only the tissue that is necessary for adequate exposure of the hip. This technique should not damage the main muscles of the hip the abductors and can be extended in any direction as needed. This is extremely important if problems arise.
Anterior approach
This is an old approach often used in childhood surgery of the hip. This technique is currently being marketed heavily in the media. Its supporters claim that muscle is not cut at the time of surgery but merely split (this may reduce post-op hospital stay and post-op pain). This is not a great issue in hip replacement surgery, rarely is pain the limiting factor for early discharge. Time to early discharge is typically more related to anaesthetic techniques such as Fast Tack Rehab than the approach used by the surgeon.
Approaches through the front of the hip may have a lower dislocation rate than a posterior approach as most but not all hips dislocate in the seated position and will dislocate posteriorly through the tissues that have been operated on. This can be significantly reducer however by a strong capsular repair in posterior approaches and limiting the tissue divided in the first place. If however the position of the hip replacement components are compromised then the dislocation rate will not be improved, another important consideration with this technique.
The main disadvantage is gaining an adequate view. This approach is very difficult to extend to get a better view if needed or deal with any unforeseen problems such as excessive bleeding. If the surgeon is having difficulty then it is possible to damage the nerve supply to the abductor muscles creating a marked limp and potential dislocation of the hip. Often the hip needs to be manipulated into extreme position to perform the technique or a special traction table is used to pull the hip apart. Unfortunately this can lead to major complications of fracture of the hip , the shaft of the femur or even of the ankle. Issues that are rarely seen in other approaches.
The complication rate from this technique appears significantly higher than with other approaches and this is especially true during the learning curve of the surgeon.If you are contemplating having an anterior approach to the hip this is an operation where it is especially important to ask the surgeon how many have you done. It may be that 50-100 hips is necessary before the surgeon has left the learning curve.
It is often claimed that an Anterior Approach to the hip results in less pain to the patient, earlier discharge, lower dislocation rates and improved patient satisfaction with an acceptable complication rate. A recent high powered study revealed non of this to be true with the only difference between an anterior approach and posterior approach from an experienced surgeon is a markedly increased risk of femoral fracture in the patients with an anterior approach.
It is for these reasons that Dr Lawrie prefers the posterior approach.
Direct Lateral approach
This is a common approach with the incision being slightly forward of the hip joint. It has a low dislocation rate as the posterior tissues are left intact. It can be done through a small incision but involves cutting through the abductor muscles. If those muscles don’t heal back onto the bone which happens in a significant number of cases then the abductors are de-functioned leading to a terrible limp which is very difficult if not impossible to correct. The incision can be extended more easily than an anterior incision but not as well as can be done through a posterior approach. There is also a significant incidence of heterotopic bone formation with this approach which results in calcification of the tissues around the hip this reduces motion and can be painful.
One of the most important issues in Hip Replacement surgery is the risk of dislocation.
Currently the risk of dislocation is about 5% for the life of the components. MIS/small incision surgery appears to give a more stable hip post-operatively as less of the soft tissues that normally stabilise the hip are cut at the time of surgery. Also the soft tissues that are cut are repaired in such a way as to impart greater stability on the hip replacement. Another potential advantage of MIS surgery is its role in revision surgery.
Follow-up surgery after a hip replacement has been traditionally very difficult. One of the major contributing factors is the degree of scarring following the initial surgery. If a less aggressive approach is used in the first surgery then it seems reasonable to think that any further surgery will be made easier if there is less scarring. Easier surgery means less complications and a better outcome for the patient. The risk of dislocation in revision surgery is above 20%, with care of the tissues beforehand then this rate may be lowered. MIS/small incision surgery cannot be employed in every case and Dr Lawrie will discuss the advantages and disadvantages of the technique and how it relates to your specific case
Surface Replacement Arthroplasty
Surface Replacement Arthroplasty has previously been popular in Australia. This is presented as a less aggressive approach to hip replacement offering a greater degree of mobility and freedom to pursue sporting activities following surgery. It has become far less popular due to a number of lawsuits following the use of particular devices as well as the unexpected failure mechanism of heavy metal reaction around these devices. DR LAWRIE HAS NEVER USED THESE DEVICES.
The advantages over a standard hip replacement are reportedly:
- The ball of the femur is resurfaced by a metal cap and stays the same size as your original ball
- Because of the size of the ball (approx. 50mm) it is more stable than a typical standard hip replacement (the ball is usually 28mm)
- There is no stem to the femoral component that passes down the shaft of the femur
- An all metal socket is typically used – having a metal on metal bearing surface Dr Lawrie is of the opinion that there are a number of problems with Surface Replacement Arthroplasty and does not offer it for the following reasons:
- The technique of putting the Surface Replacement Arthroplasty in your hip is more difficult than a standard or MIS Hip Replacement.
- It is conserving of bone on the femur but takes a little more bone off the socket in the pelvis.
- The biggest problem with long term survival of Hip Replacements is the longevity of the socket not the ball and stem. The socket is much harder to put in with Surface Replacements, if the position of the socket is not right then the survival of the socket is reduced. The harder it is to do then the more likely a problem will occur.
- If the position of the socket is not exact then major wear problems can occur. It was originally thought that these implants would be more forgiving of malpositioning, unfortunately the opposite has occurred and the survival of these devices is critically affected by small changes in alignment.
- Surface Replacement Arthroplasty takes away more bone on the socket side so as to be able to cover the large ball. This leaves less bone for subsequent surgery if required, also potentially reducing the bone stock that the current socket has to support it.
- There does not appear to be any problems with putting a well designed stem down the centre of the femur as in a standard hip replacement.
- If the ball is not aligned perfectly there is a risk of fracturing the neck of the femur. This happens in about 5% of cases. If this occurs then a normal hip replacement can be placed in the femur but the socket needs to be replaced also. This is a problem since the socket will not be loose and already a large amount of bone has been removed, making a very difficult socket revision.
- A much larger approach is needed than MIS. At the time of revision surgery there will be much more soft tissue damage making the surgery harder and the risk of complications such as dislocation higher.
- Early failures (within the first five years) are reported even in the best series. This risk is substantial.
- Revision of standard hip replacement components although not perfect is well understood and there are good fall backs in the case that further surgery is necessary.
What to do when a Surface Replacement Arthroplasty needs to be revised is not well understood and there are not well designed components to handle this type of revision.
- Metal on Metal bearing surfaces release heavy metals into the systemic blood supply. Cobalt levels have been shown to continue to rise for many years following this type of surgery. Cobalt can cause kidney failure, heart failure and potentially cancer. We will never be able to prove or disprove a cause and effect of cancer due to the extremely large numbers needed to prove this.
- Metal ions can also have a profound but poorly understood affect on local tissues. A problem called ALVAL can occur which is a massive soft tissue reaction (so called pseudo-tumour) about the hip can form in response to these metal ions. Large soft tissues masses can form which are very difficult to treat.
- Certain patients should definitely not have surface replacements Patients over 65yrs, patients with osteoporosis, patients with major deformity and patients with small sockets all do much worse with surface replacement over traditional total hip replacement.
- There is no evidence that surface replacement patients have better function, range of motion or higher activity levels than modern total hip replacement surgery despite the many marketing claims to the contrary.
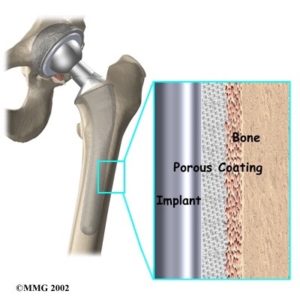
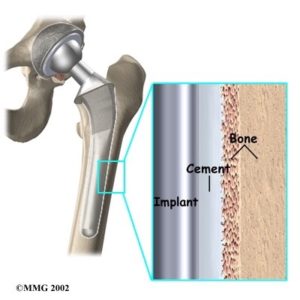
Cemented Or Uncemented Hip Replacement
This describes the type of fixation used to secure your hip replacement to your bone. Traditionally hip replacements have been performed with cement. Bone cement is an acrylic compound – polymethylmethacrylate or PMMA. Bone cement acts like a grout to lock into the small spaces within the porous bone cavity. It acts to transfer stresses from the component to the bone in a controlled way.
A cemented THR will suit a large percentage of typical patients requiring a THR. There is some concern that in young and or very active patients the fixation of cemented THR may not be as durable as uncemented THR. There are certain hips where a cemented THR is more advantageous then an uncemented hip.
Patients with inflammatory conditions such as Rheumatoid Arthritis, patients with osteoporosis and patients with a stove pipe shape to their femur do better with a cemented implant. Uncemented THR emerged in North America over the last twenty years due to the partially mistaken belief that cemented hips wear out due to the bone cement itself. Uncemented hips are usually made of titanium, which is very biof-riendly to bone. The surface of these implants is rough. They gain fixation by getting an immediate mechanical interlock with the rough surface and then the bone grows into the surface of the implant over time.
Certain hips are better suited to uncemented THR, especially if the patient has a particularly narrow femur, young and/or active patients probably are better suited to an uncemented THR.
Bearing Surfaces
The bearing surface describes what the actual ball and socket are made out of. Traditional THR has a metal alloy ball and a plastic socket. With the socket either cemented into place or in uncemented in a metal shell. One of the main reasons hip replacements wear out is due to wear of the plastic liner.
As the plastic wears, particles are released which produce an inflammatory reaction around the implant, which can damage the bone and lead to loosening of the hip. We know that the plastic in the socket does wear out over time, but this is still usually a very gradual process and in a large majority of patients is not relevant due to the patient’s age at the time of initial surgery. However in young patients or it the very active this wear can be accelerated and lead to failure of the THR. This has lead to the recent introduction of a number of newer bearing surfaces to address the issue of wear.
The following changes have occurred;
1. New sterilisation procedures – Previous problems with accelerated wear of the plastic component occurred at least in part due to the way the plastic was sterilised. Modern sterilisation has prevented oxidation of the plastic, which caused accelerated wear. Therefore standard plastic liners are now more resistant to wear than previously and often very good wear characteristics, which will suit most patients. The advantage of using traditional plastic is that we know how this plastic wears, acts and performs better than any other bearing surface. Also plastic liners can be manufactured into a number of different options allowing better mechanical function of the THR.
2. Newer Plastics – Because traditional plastic does wear over time, a new plastic has become available. By irradiating the plastic when it is sterilised the plastic becomes much harder and resistant to wear. Laboratory studies show excellent levels of extremely low wear rates with this plastic known as Cross-Linked Polyethylene. There is some concern that this plastic may be more brittle than traditional plastic and that the wear particles that are created may be more active and create greater levels of inflammation then traditional plastic. Cross-linked polyethylene is now the most common alternative bearing used at present and to date no problems have been encountered to any great degree, There are now a number of studies showing excellent results to ten years and beyond with these bearing surfaces.
3. Metal on Metal Bearings – These components use both a metal head and a metal socket as a bearing surface. Early hip replacements were performed with this type of bearing but it disappeared due to the more user friendly metal on plastic components. However it was observed that these older metal on metal bearings have lasted for 30yrs or more with the surfaces still looking very smooth. This has lead to resurgence in metal on metal technology.
The main advantages of metal on metal bearings are:
- A larger ball can be used which gives better stability, hence lower dislocation rates,
- Very low wear rates
- The metal does not fracture like ceramics may do. The disadvantages are:
- The release of fine metal particles into the blood stream.
- Cobalt is released from the bearing surface over time.
- Cobalt is a heavy metal.
- At certain blood levels Cobalt can cause damage to the kidneys and heart and may cause chromosomal changes.
There is no evidence that these problems occur in THR patients but we need very large numbers of THR patients in a study to prove any problem. It is not possible to run a study of this size. Therefore there will always be a question of whether metal on metal bearing surface cause a problem to the kidneys, heart of even cancer. For this reason they should be used with caution in younger patients or patients of child bearing age. The certainly have a distinct advantage in the patient who is prone to dislocation as a bigger ball can be used. These are the same bearing surfaces as in surface replacement and could suffer similar problems. Positioning of the socket is not as difficult however when used as a hip replacement compared to a surface replacement.
Oxinium
Oxinium is a new alloy which, when heated, in an oxygen rich environment develops a surface layer which acts like a ceramic. It is extremely smooth and wear resistant as well as slippery but still retains the mechanical qualities of an alloy. Therefore it will not fracture like a brittle ceramic. Oxinium is very useful as a bearing surface on the ball side but it can’t be mated to a socket of oxinium. It has to be used with a plastic socket.
Therefore you still have the problems with the plastic socket of wear but it appears to be much reduced with oxinium (whether the plastic is cross-linked or not). Oxinium has now been in use for about ten years. I am not aware of any research showing problems in the hip with oxinium and it shows great promise. The Australian Joint Registry is showing excellent results with Oxinium as a bearing surface. At present it is only available from one company and can not be used in other company’s hips.
Ceramics
Ceramic components have been used for about thirty years in Europe but only in very limited numbers in North America as they have only recently gained FDA approval (2002). Ceramics have the lowest wear rate of the alternative bearings.
- The particles produced are relatively inert – they do not produce much of an inflammatory reaction and hence little resorption of bone.
- They can come in larger head sizes so are more resistant to dislocation.
- They have been used in large numbers in Europe for many years and so there is a large body of literature available.
- Ceramic particles cause no problems to other organs such as the kidneys or heart.
- They do not cause cancer.
- However ceramics are brittle; they fail when they fracture.
- Ceramic bearings offer the lowest wear rates of any bearing surface, this may be very useful in the young patient. If there are any impurities in the ceramic then the chance of fracture dramatically increases. In 2000 there was a world wide recall of ceramic components made by one particular French manufacturer due to a problem in production techniques. The current ceramics used are produced at one company and are very carefully tested to avoid the problems previously encountered. The current quoted fracture rate is 1 in 10 000 THR’s. This should be a very uncommon occurrence.
When a ceramic component fractures it is an immediate event. It can feel like the hip explodes as apposed to a metal on plastic which gradually fails over time. However the number of hips which fail should be much less than a metal on plastic hip. When a ceramic THR fractures it is very difficult to revise due to the presence of fragments of the ceramic that may be left. Traditional results of revision surgery are relatively poor for ceramic failures.
One can argue that you should revise a ceramic hip with another ceramic hip. This can be technically very challenging. The chances of fracture of a ceramic are higher when there is a problem with impingement of the hip or dislocation. If there is unusual anatomy of the original hip then this can lead to problems with the ceramic hip. Impingement is when the edge of the cup abuts on the neck of the femoral component. This can lead to levering out the head from the socket resulting in chipping and eventually fracture of the ceramic. Therefore if there is unusual anatomy or a high risk of dislocation it may be best to avoid ceramics. Squeaking of the ceramic liner can also be an issue.
This can be due to impingement or due to lubrication issues. Sometimes a squeaking hip results in further surgery and repositioning of the socket and/or exchange of the liner. Ceramics do not have the variety of components that are available with metal on plastic bearings and so the surgeon does not have as many options with this bearing surface. There is no bearing surface that is perfect at present. Each has their advantages over the next, but there is also a down side to all of these emerging technologies. They each have their place and a decision is made on an individual basis, depending on the patient’s particular requirements. What all of the above allows is for a custom hip to be devised to suit the individual patient’s needs and hence get the best result out of their new hip replacement.
Head size
In the last few years there has been a move to using larger head diameters in total hip replacements. This has been possible due to the better wear characteristics in the newer bearing surfaces. Originally the head or ball of the femoral component measured slightly greater than 22mm’s as it was felt that this produced the lowest wear on plastic sockets. Over time larger heads were introduced 26mm heads then 28mm heads were used. 28mm Heads have been the standard size for the last 20years or so. Recently larger heads 32mm commonly 36mm with ceramic and even to 40mm and beyond have been used.
With metal on metal implants the bigger the head the less wear but with ceramics and plastics there has been concerned that bigger heads may create problems with accelerated wear. Recent evidence is now showing that larger heads are doing better than 28mm heads as long as there is enough material in the socket to cope. Larger heads will be more stable and hence fewer dislocations should occur and as long as the correct size head is used for the corresponding socket and type of bearing surface increase wear hasn’t been a problem. In very small hips 28mm heads will still need to be used. From all of the above information it can be seen that various options are available to suit your needs and a hip replacement can be “tailored” to the individual characteristics of each patient.
Download