Please read this document in conjunction with the ACL injury pathway and the ACL reconstruction pathways.
There are a number of options with regards to ACL reconstruction surgery, each have there advantages and disadvantages. There is no one ideal way to reconstruct a torn ACL nor is every knee with a torn ACL the same. The following explains the pros and cons of each technique. I use an individual approach for each patient depending on their needs and injury, hence customising surgery to the individual. This is based on over 15 years of personal experience as well as visiting and training with many world leaders in ACL surgery and attending many major international meetings on the subject. I have performed each of the techniques described here and made my own judgements on their benefits and disadvantages taking into consideration the current literature.
The goal of the ACL surgeon is to prevent further instability about the knee, which results in more damage, and to preserve meniscal function and articular cartilage. Typically the goal of the ACL patient is to return to sport or a high level of function.
The options available in ACL reconstruction surgery can be considered as;
- ACL graft options
- Meniscal repair options
- Articular cartilage preservation techniques
- Extra-articular procedures
- Rehabilitation options
GRAFT OPTIONS
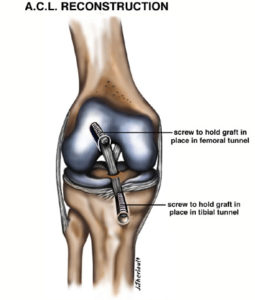
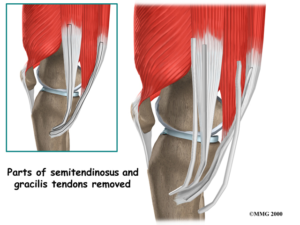
Hamstrings
Most common graft choice in my hands. I typically use Gracilis and Semitendinosus tendons from a small incision on the inner side of the knee. A special tendon stripping device is used to harvest these two tendons from their muscle belly. The length and thickness of the tendons is quite variable. The two tendons are typically folded over and sutured top and bottom to produce a 4-strand graft. The graft needs to be of a reasonable length and thickness to allow adequate fixation and graft strength. Many surgeons aim for a graft at least 8mm thick (this may not be necessary for everyone but is a common starting point). The position of the bone tunnels through which the graft is passed and secured is critical to the end result.
Advantages
- Common technique
- Easier rehab than BPTB
- Anterior knee pain is not an issue
- No weakness for jumpers
- Maybe less arthritis than BPTB
- Kneeling is not a problem
- Safer in children with open growth plates (depending on fixation method)
Disadvantages
- May have higher re-rupture rate than BPTB
- A study from New Zealand reports significantly higher rates of re-rupture in teenage girls compared to BPTB
- Sometimes quality of tendon is marginal
- Difficult to harvest
- May have some hamstring weakness (usually not significant)
- May “stretch” compared to BPTB.
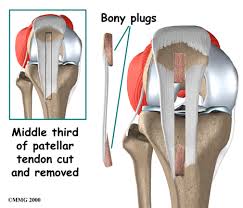
Bone Patella Tendon Bone (BPTB)
The most common alternative to hamstring graft is the Bone Patella Tendon Bone graft or BPTB graft. This involves taking the middle third of the patella tendon (the tendon joining the kneecap to the tibia/shin bone) along with a block of bone at each end of the tendon where it attaches to the patella and tibia
Advantages
- Easier to harvest as it is sitting at the front of the knee
- May be stiffer, stronger than hamstrings
- May have lower re-rupture rate than hamstrings in certain patients (teenage girls)
- Bone block at top and bottom of graft is very useful in revision surgery for filling wide tunnels
Disadvantages
- Anterior knee pain is not uncommon
- Difficult kneeling on the scar (especially for tradesman)
- Bigger thicker scar on the front of the knee
- Can be harder to rehab in older patients
- May have higher incidence of osteoarthritis
- Can be difficult to return to jumping sports
Hamstring patients tend to reinjure the same knee, BPTB patients tend to injure the opposite knee. Both groups tend to return in similar numbers.
Quadriceps tendon
Occasionally the quadriceps tendon, above the patella, can be used. Like the BPTB graft a bone block of patella is taken but neither bone block is superior. This graft is rarely used in ACL reconstruction but it can be useful at times.
Advantages
- Can be used in revision surgery of hamstrings when the BPTB or the opposite hamstrings can’t be used. E.g. patient has had Osgood Schlatters disease or a tibial nail inserted through the patella tendon insertion.
- Can be a large/wide graft.
Disadvantages
- Can be difficult to regain quadriceps function during rehab
- Can be a flat tendon and delaminate which doesn’t match the normal geometry of the native ACL.
- Scar can be unsightly.
- Tendon may be surprisingly short at times.
Iliotibial Band (ITB)
Is a strip of tissue on outside of knee. Can be harvested in a similar way to a hamstring harvest. The ITB is not used as a graft on its own but is useful to bulk up a thin hamstring graft.
Advantages
- Increases size of a thin hamstring graft
- Relatively easy to harvest.
- Of very similar tissue to hamstrings so quite easy to incorporate with hamstring tendons.
- No extra-cost to use and takes little time to add to hamstrings.
Disadvantages
- Extra-scar on outside of knee.
- Can be of variable length and quality.
- Can leave a gap in tissue on outside of thigh
- More painful.
Allograft
Allograft tissue is tissue obtained from the bone bank from deceased patients who donate their organs. A variety of materials can be ordered, different tendons, ligaments, BPTB, tibialis anterior tendons etc.
Advantages
- Ease of use
- Can have any type of graft needed
- Size is not an issue
Disadvantages
- Very costly
- Variable quality and availability of graft
- Very low risk of disease transmission
- Takes twice as long to reach necessary strength
- Significantly higher failure rate especially early on
Short Graft TLS system
This is a relatively new way of using the hamstring tendons for the an ACL graft. The technique uses a tape screw fixation device that allows the graft to be much shorter than traditional techniques. The graft still needs to be put in the same place as traditional techniques but only needs to be 50-60mm long instead of 120mm. The tunnels are made with hand reamers rather than using a power drill which may reduce bone pain.
Advantages
- Thicker graft (thicker is stronger).
- Can always produce a graft >8mm

- Good option if hamstrings are of marginal quality
- May have less pain
- May need only one hamstring tendon
- May be a little easier to rehab
- May have less tunnel widening
- May be easier to revise
Disadvantages
- Thicker graft may not always be best (large grafts may not fully transform into a healthy ligament)
- If very thick graft revision may need to be done as a 2 stage procedure
- Cost especially in uninsured patients
- Have to remove all of native ACL so can’t preserve ACL remnant
- Complex fixation device, more room for error
- Is not widely used so it does not have same volume of evidence to support its use
Remnant preservation/Repair
This is a particular interest of mine. I have devised a technique to repair the native ACL.
In some circumstances although the original ACL has torn there may be substantial tissue remaining which can be preserved. If there is ACL tissue from top to bottom then that tissue can be saved and incorporated into the ACL graft. A graft is still prepared using the 4 strand hamstring technique and this graft is passed through the original ACL and fixed as usual. The original ACL is repaired back to the femur. This creates a graft/ACL composite.
Advantages
- Preserves some of the original ACL
- Maintains the blood supply of the original ACL so may produce more rapid or improved ligamentisation of the graft
- Maintains the nerve supply of the original ACL especially proprioceptive fibres. Proprioception is position sense of the joint and this is what we are trying to restore in ACL surgery.
- May improve rehab ability because of maintained proprioceptive fibres.
- Produces a large graft/ACL composite structure.
- Seals off the tibial tunnel reducing the chances of graft impingement and scar formation.
Disadvantages
- Very difficult technique
- ACL surgery is about getting the femoral and tibial tunnels in the correct position. If the technique is more difficult or vision is obscured e.g. by the graft remnant than this may lead to tunnel placement issues.
- Needs specialised equipment
- Only suitable in a small percentage of patients 10-20%
- Repaired original ACL may not heal and may scar and impinge instead
Living Donor Graft
In very rare situations it may be possible/worthwhile for a parent to donate their hamstrings as a graft for their child. Very young children may have inadequate tissue for an ACL graft. This is more likely in the revision situation or when an allograft is inappropriate.
Advantages
- Allows for a bigger graft in the very young.
- Does not weaken the hamstrings in a young growing patient.
- Avoids the risks of an allograft in young patients.
Disadvantages
- Requires considerable planning including pre-approval from the hospital ethics committee, which can take some time.
- Need to ensure the donor tissue is blood type compatible with the patient.
- May take longer to incorporate (like an allograft).
- There is a risk of disease transmission.
LARS
The LARS is a polyester artificial ligament augment or replacement device that can be used instead of a traditional biological graft (e.g. 4 strand hamstring graft). The LARS technique had a surge of popularity several years ago due to its use in some high profile athletes, but then suffered a significant decline in popularity after some high profile re-ruptures. Currently the Australian Knee Society cautions the use of this device.
Advantages
- Immediate strength is obtained.

- Accelerated rehab possible at 3-4months.
- Can be a “get out of jail” technique in extreme situations
Disadvantages
- Still has a failure rate
- Need a “healthy ACL remnant” for LARS to support
- If used outside of strict indications LARS has a higher failure rate
- When fails can be incredibly difficult to revise often requiring a 2-stage procedure
- Concerns about the long-term consequences of artificial tissue in the knee
- Other artificial grafts have created huge synovial reactions but this has not been seen as much with the LARS device
ITB tenodesis
Some patients are at high risk of re-rupture following their ACL reconstruction. Patients with marked rotation at the knee or with ligamentous laxity are at particular high risk. Young females often have these characteristics. In these situations the addition of an extra-articular tenodesis can act as an internal splint and reduce the rotational forces on the ACL graft to improve stability and hopefully reduce re-rupture rates. A strip of the ITB can be harvested in a similar way to the hamstring harvest, then passed under the lateral ligament and reattached to either the femur or the tibia creating a loop of tissue on the outside of the knee.
Advantages
- Reduces rotational loads on ACL graft
- May reduce re-rupture rates in high risk patients
- At the end of rehab doesn’t reduce the range of motion
Disadvantages
- Complex technique
- Bigger operation
- More pain and stiffness at least at the start of rehab
- Slower and more difficult rehab
- Need to be careful of growth plates in young patients
MENISCAL REPAIR OPTIONS
Preserving meniscal function is key to a successful long-term outcome. I will always repair the meniscus if at all possible. Studies show that if a meniscal tear is present early surgery to repair the meniscus best preserves the meniscus. The technique of repair depends on the nature of the meniscal tear and its anatomical location.
Fast-Fix 360 device
This is the device I use most commonly for meniscal repair. It is a preloaded suturing device which deploys two small anchors through the meniscal tear into the knee capsule. The anchors are connected by a suture with a hand-tied sliding knot.
Advantages
- It is “all Inside device” so there is no need for a separate incision to tie the knot. Because of this it is much less likely to cause an injury to structures behind knee.
- The knot is tensioned under direct vision to avoid an overly tight repair.
- The needle used for the repair can be bent to manipulate the torn fragment into place.
Disadvantages
- Cost is the major one, each device costs about $460 and typically I use about 4 per torn meniscus.
- It can leave a larger hole in the meniscus than inside out sutures.
- About 5% technical failure rate as it is a hand tied complex device
Best suited for tears at the back of the knee where the majority of tears are. It is also more useful for complex tear patterns as the meniscal fragments are more easily manipulated and tension more readily controlled.
Inside Out Suture
This is the original suture device. This device is a suture with a very long needle at either end. Special suture passers are used to deliver the needle arthroscopically across the tear and then the needle is passed from inside the knee through the meniscus and out through the capsule and skin. A separate incision is made on the outside of the knee and the sutures are traced back to the capsule and then knotted over the capsule.
Advantages
- Inexpensive
- It leaves a smaller hole in meniscus than the Fast-Fix 360.
- Very useful to reduce bucket handle tears
Disadvantages
- Difficult to protect the structures behind the knee when suturing behind the knee.
- Need a separate incision on the outside of the knee to tie the suture.
- Difficult to manage multiple sutures as all sutures have to be passed before tying the knots.
- Higher risk of nerve injury.
- Difficult to tension the suture as the knot is tied to the capsule rather than on the meniscal tear.
Is best suited for bucket handle tears and tears in the mid section of the meniscus.Often used in conjunction with Fast-Fix 360 sutures placed posteriorly in the meniscus.
Outside In Suture Kit
This technique involves placing a pair of hollow needles across a meniscal tear from outside the knee through the torn meniscus and then into the knee. A suture is then passed up one hollow needle and then back out the other and then the suture is tied on the outside of the meniscus.
Advantages
- Only technique for anterior horn tears (these are uncommon)
- Inexpensive
- Can angle the sutures differently to sutures passed from inside so can be useful in some angle tears
Disadvantages
- Quite difficult to master
- Needs a separate incision so it may cause a nerve injury.
- Leaves a bigger hole in the meniscus
Root repair technique
The root of the meniscus is the very anterior or posterior attachment of the meniscus to the tibia.In ACL injury the root of the meniscus is commonly damaged. While this can appear to be a subtle injury arthroscopically it is devastating for the knee and must be repaired if present. This requires a different technique; usually 2 or 3 Fast-Fix 360 sutures are placed in the root of the meniscus securing the knot into the meniscus but instead of cutting the suture flush with the meniscus the tail of the suture is left long, the meniscus is moved into place and the suture is secured with the ACL graft in the tibial tunnel at the end of the operation.
Advantages
- Preserves the root of the meniscus
Disadvantages
- Difficult technique
- Need to be careful with sutures placed near the midline to avoid injuring nerves and vessels behind the knee
CARTILAGE OPTIONS
Micro-Fracture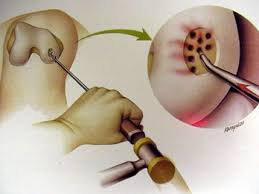
The most common technique for full thickness cartilage injuries of the joint surface. The technique involves debriding a cartilage defect back to a stable rim and using a special instrument (much like a fine ice pick) to puncture multiple holes in the base of the defect at a certain depth and distance. This creates a blood supply to the defect, which transforms from a blood clot to fibro-cartilage over 3-4 months. The cartilage is quite robust following this but the repaired cartilage is never returns to normal cartilage.
Advantages
- Simple, inexpensive procedure
- Works particularly well on the medial and lateral femoral condyles not so well elsewhere
- Works best in small defects
Disadvantages
- Patients need to be non-weight bearing for at least 6 weeks
- Poorer results when there is a large defect or there is a defect in the patella-femoral joint.
- Cartilage in-growth is fibro-cartilage not hyaline cartilage so this new cartilage will probably deteriorate over time
PRP Platelet Rich Plasma
PRP can be used to enhance the results of micro-fracture in difficult situations. PRP may improve cartilage ingrowth after micro-fracture in difficult situations such as large defects and patella-femoral defects.
Advantages
- May improve cartilage in micro-fractured knees as above
Disadvantages
- Increase complexity of procedure
- Needs to be repeated post-operatively
- PRP interacts with a number of medication including anti-inflammatory medications
- Limited research available on this technique
- Increases costs as it is not rebateable at present
- Needs specialised equipment in the operating theatre
REHABILITATION OPTIONS
Your post-operative rehab coarse is a major determinant of how good the knee will be at the end of the day. I consider that 50% of the final outcome is due to what happens at the time of surgery and 50% due to what happens during rehab. One can’t compensate for the other; both need to be optimised for a successful outcome.
In general there are a number of stages of rehab;
Pre-op From injury to surgery
Stage 1 0-2 weeks, the goal is to reduce the pain and swelling
Stage 2 2-6 weeks, the goal is to protect the meniscal repair, micro-fracture etc.
Stage 3 6-12 weeks, the goal is to ensure full range of motion. This is achieved through closed chainbody weight strengthening exercises and proprioception exercises
Stage 4 12-26 weeks, the goal is to improve strength. This is achieved through gym/resistance work, jogging swimming, return to manual work
Stage 5 26-36/40 weeks sports specific training, landing, change of direction exercises
Stage 6 Formal Return to Sport assessment including fatigue testing and MRI assessment
Very commonly a rehab programme is produced as a set of exercises that if followed will result in a successful outcome. They read like a recipe or cookbook that if followed will result in a good outcome. However every patient is different and there are many variables as described above which have a major influence on ones rehab.
The age of the patient, the time the patient can put into their rehab, work requirements, the quality of the articular cartilage and subchondral bone, type of meniscal injury and or repair, type of graft all impact and change the rehab process.
As the rehab programme progresses and the load on the knee increases it is very important that the knee has settled from a pain, swelling, range of motion point of view before load is increased. So the rehab process is individualised for each patient and their injury. The final stage of the rehab programme is a formal return to sport assessment to ensure the patient and the knee is ready to return to full activities, again this is a particular interest of mine and we have been conducting research into this area for a number of years.
CONCLUSION
The goal of treating ACL injuries is to stabilise the knee and to protect the menisci and joint surfaces to allow/ensure a safe return to sport (or work) whilst minimising the risk of further injury. There is no single technique that has proven to be the best due to the number of variables at play. For every patient I consider the known advantages and disadvantages of the techniques outlined here to deliver a customised, targeted approach that, in my hands, will produce the best outcome for the individual. This is customised ACL surgery.
